Cataracts in dogs
What are the causes of cataracts in dogs?
Cataracts in dogs most often develop as a consequence of diabetes (D. mellitus). Almost 90% of diabetic dogs develop cataracts in the first 12 to 18 months of diseases onset. In many breeds of dogs, cataracts are hereditary (congenital cataracts). Some dogs are born with hereditary cataracts, while others develop cataracts as they age. Cataracts can also occur as a result of trauma or inflammation.
What is a cataract?
A cataract is a clouding of the eye lens or its sheath (lens capsule) of varying degrees, from mild to complete opacity, resulting in reduced vision.
Should we be worried if our pet is diagnosed with cataracts?
When cataracts are diagnosed, it is very important to identify the cause that led to the cataract as well as to monitor the progression of the cataract. A lens affected by cataracts constantly leaks lens content material, which can be very irritating and harmful to the eye. The material which leaks from the lens is recognized by the immune system as foreign material, so aggressive autoimmune reactions can develop, resulting in pain, vision loss, and eventually eye loss.
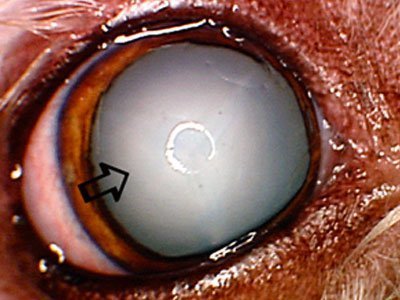
A cataract is an abnormal change in the composition of the lens, which results in a white, milky appearance of the lens (arrow). Sometimes diabetic cataracts progress rapidly over weeks or even days, resulting in sudden blindness. Rapidly progressive cataracts can be very harmful due to the inflammation and irritation they cause, and in some cases can result in the development of acute glaucoma. If you notice a weakening of your pet’s vision or the appearance of a milky white eye, contact your veterinarian immediately.
Cataracts can change, and progression from small opacity to complete clouding of the lens can happen over a short period of time (several days), or a long period (several months or years). Any rapidly progressive cataract should be considered an emergency condition of the eye, and an ophthalmologist should be sought immediately. Small cataracts, which do not cause significant eye irritation or visual disturbance, are usually only monitored. Cataracts that cause significant vision problems or eye irritation must be surgically removed to restore vision and reduce the risk of possible eye loss associated with uncontrolled eye inflammation. Due to the numerous complications associated with cataracts, it is important to medically treat and monitor cataracts in all cases in which surgery is not performed. Medical treatments usually include topical anti-inflammatory eye drops that are applied once or twice a day. In some cases, systemic anti-inflammatory drugs may be required.
Complications associated with cataracts
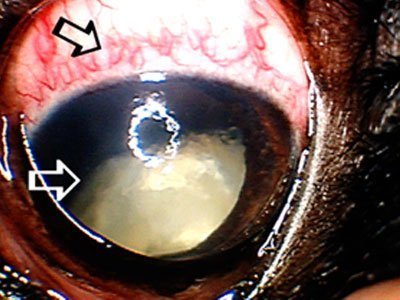
The prolonged presence of cataracts can cause a number of complications that may eventually require surgical removal of the eye. This patient had cataracts (white arrow) for a long period of time, which resulted in glaucoma (increased intraocular pressure), pain, and redness of the eye (black arrow).
How is a cataract treated?
Cataract surgery is a routine procedure performed by veterinary ophthalmologists that is 95% successful. The amount of money spent on cataract surgery is equal to the amount of money invested in medical treatment over a period of 3-5 years in cases where surgery was not indicated. By performing cataract surgery, the patient’s vision is restored and the chances for the appearance of numerous complications are dramatically reduced.
What are the possible complications associated with cataract surgery?
Complications that can occur due to cataract surgery are very rare. The most common complications of cataract surgery are glaucoma (development of increased intraocular pressure), retinal detachment, and severe intraocular inflammation or infection. These complications can be remedied with aggressive medical treatment, but in some cases, an additional surgical procedure may be required to ensure a good outcome.
What can be done to prevent surgical complications associated with cataract surgery?
Your ophthalmologist will perform a detailed assessment of the eye before cataract surgery to identify potential problems (intraocular inflammation, predisposition to glaucoma, possible abnormalities in the function and structure of the retina). It is very important to clean the teeth before the surgery so that after the cataract surgery, an intraocular infection with teeth bacteria can be prevented. Many diabetic dogs have urinary tract infections (due to the presence of glucose in the urine), so they should be given systemic antibiotics prior to cataract surgery.
Does cataract surgery need to be repeated?
Cataract surgery is performed only once. At that time the lens affected by the cataract is completely removed and an artificial lens is placed in the eye.
Is there a problem if an artificial lens is not placed in the eye during cataract surgery?
In rare cases, an artificial lens cannot be placed in the eye, which can result in poorer vision in some dogs, while most dogs have almost normal vision. Dogs without an artificial lens usually have trouble seeing small objects near their eyes.
Artificial lens
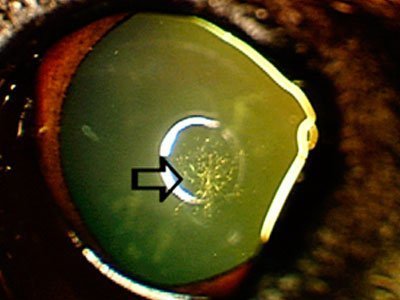
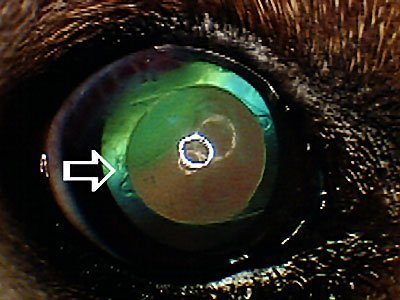
Cataract surgery is a reliable method of permanent removal of cataracts and restoration of normal vision. An artificial lens (white arrow) is usually placed in the eye to improve vision. Cataract surgery eliminates the risk of chronic inflammation caused by cataracts as well as the occurrence of many other complications (retinal detachment, glaucoma, intraocular bleeding).
I can’t afford cataract surgery – what are my options?
Cataract surgery requires a significant financial commitment, and if resources are not available to perform cataract surgery, it is necessary to conduct a local (and in some cases systemic) anti-inflammatory therapy. Unfortunately, the progression of cataracts is always associated with many complications (secondary intraocular inflammation, lens luxation, intraocular hemorrhage, secondary glaucoma) which ultimately dictate the need for surgical removal of the eye.